
Diagnosis Information
Receiving difficult news about your baby in the Neonatal Intensive Care Unit (NICU) can be one of the most overwhelming moments of your life. As a parent, you may feel a flood of emotions—fear, sadness, confusion, or even numbness. It’s completely normal to struggle with processing unexpected diagnoses, but you are not alone. Here, you'll find information on diagnostic conditions and medical terms that may affect your baby. This resource is for informational purposes only and should not replace medical advice from your baby's NICU care team.
Brain Bleed (Intraventricular Hemorrhage)
There are several different types of bleeding that can happen in a premature baby's brain, the most common is intraventricular hemorrhage (also referred to as "IVH") which is what is discussed here.
Why does it happen?
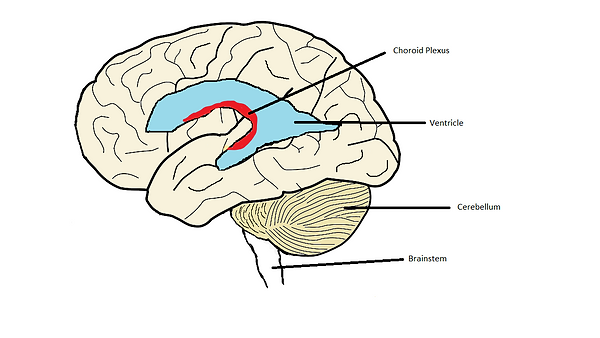
Premature babies are at risk for bleeding in the spaces inside their brain called the ventricles (see the figure at the bottom of this post). There are very fragile blood vessels within the ventricles that can easily break and lead to bleeding. You baby will likely have a head ultrasound within the first few days of life (similar to the ultrasounds that were done during pregnancy, so no radiation and no significant stress on the infant) to look and see if there is any bleeding. This will be done at the bedside and uses the anterior fontanelle, or soft spot, on the top of the baby's head to get a view of the brain. If any bleeding is seen, your baby's doctors may want to get another head ultrasound in a few days to monitor the bleed and make sure it is not getting worse.
What is the treatment?
Initially, your baby's doctors will watch your baby very closely and make sure that the bleeding has stopped; this is done by getting ultrasounds of your baby's brain. With small bleeds, your baby's brain will be able to get rid of the blood on their own once the bleeding has stopped and nothing further with need to be done. If your baby has a very large bleed, your baby will probably get frequent head ultrasounds to monitor the size of the ventricles. Sometimes, the brain is not able to get rid of the blood because there is so much and this may cause the ventricles to get bigger. If this happens and the ventricles continue to grow in size, your baby may be diagnosed with hydrocephalus which means increase size of the ventricles. Depending on the size of the ventricles, your baby may need a sugery (often many weeks later once they have grown much larger).
What are the long term effects of IVH?
That depends on how big the bleed is. The radiologists (doctors who specialize in reading, xrays, ultrasounds, MRIs, CTscans etc) that look at the images of your baby's brain will grade the degree of bleeding.
There are 4 grades:
-
Grade 1. Bleeding occurs just in a small area of the ventricles.
-
Grade 2. Bleeding also occurs inside the ventricles.
-
Grade 3. Ventricles are enlarged by the blood.
-
Grade 4. Bleeding occurs in the brain tissues around the ventricles.
Grades 1 and 2 are most common and often these babies have no long term complications. Grades 3 and 4 are the most serious. Because these bleeds can affect the brain tissue, they may result in long-term brain injury. This can't be determined while your baby is in the NICU and so it is really important that your baby is followed closely by their pediatrician as well as either a pediatric neurologist or pediatric neurodevelopmental specialist.
Congenital Heart Disease
How does the normal heart work?
There are 4 chambers in the heart, 2 upper chambers called the right atria and left atria and 2 lower chambers called the right ventricle and left ventricle. Blood comes from the body and goes into the right atria. It then flows through the tricuspid valve into the right ventricle where it is pumped into the lungs to get oxygenated through the pulmonary artery. After traveling through the blood vessels in the lungs, the blood returns to the heart through 4 pulmonary veins in to the left atria. From the left atria, the blood goes into the left ventricle through the mitral valve and then gets pumped out to the body through the aorta. This cycle repeats itself with every heartbeat. (see diagram below). www.cdc.gov/ncbddd/heartdefects/facts.html
Below you will find some examples of different types of congenital heart disease. Congenital means that this problem occurs during the development of your baby early on in pregnancy. At the end, you can find links to different sites that have additional information.
Hypoplastic Left Heart Syndrome (HLHS)
What is it?
This is a congenital heart defect where the left side of the heart didn't develop normally. Remember, as described in the section on how the normal heart works, the left side of the heart pumps oxygenated blood through the aorta to the body. There are 3 main defects, or problems, in babies with HLHS: The first is that the mitral valve that separates the left atria and the left ventricle is too small or closed; the second is that the left ventricle is underdeveloped and very small, and the third is that the aortic valve is very small or not present (like the mitral valve) which leads to underdevelopment of the aorta. These defects lead to decreased blood to the body and if not corrected will lead to death.
(Diagram of HLHS)
How is it treated?
The good news is that in the 1980's a surgery was developed to help fix the problems seen in this congenital heart defect; the surgery is done in 3 stages. The pediatric cardiologist and the pediatric cardiothoracic surgeon will go over in detail how the surgery will be performed; and remember there may be small differences in how the surgeon will do the surgery if your baby's HLHS has slight differences or variations in the defect compared to the typical baby with HLHS. So briefly, there are 3 stages to fixing HLHS which will create normal blood flow into and out of the heart to the body can get the oxygenated blood that it needs to survive.
1. The first stage is called the Norwood procedure (named after the surgeon who developed it). This surgery will usually be done within the first week of life. In this initial surgery, the right ventricle is converted into the main ventricle that will pump blood to the body (essentially doing what the left ventricle would normally do). This is done by using the pulmonary artery (the vessel that connects the right ventricle to the lungs) and attaching it to the aorta that is underdeveloped so it essentially creates a new aorta. So now the blood from the right ventricle can go out into the body. But how does the blood get into the lungs to be oxygenated now? This is done by using a special tube, called a BT shunt, that connects the right pulmonary artery to one of the vessels that connects to the aorta. So what this does now is when the blood goes out from the right ventricle through the new aorta some of the blood will go to the body and some of the blood will go through the BT shunt to the lungs to be oxygenated.
(Diagram of Norwood procedure for HLHS)
2. The second stage, or second surgery for HLHS, is called either the hemi-Fontan or bidirectional Glenn procedure.
(Diagram of hemi-fontan procedure)
3. The third stage is called the Fontan procedure.
(Diagram of the Fontan procedure)
Tetralogy of Fallot (TOF)
Transposition of the Great Arteries (TGA)
Ventricular Septal Defect (VSD)
This is the most common type of congenital heart defect. A VSD is a hole in the wall, or septum, of the lower 2 chambers of the heart (the right and left ventricle). They can range in size from very small to large. When a VSD is present, it allows blood from the left side of heart to flow into the right side of the heart which increases the amount of blood that goes into the lungs. The extra blood that is going into the lungs causes the heart and lungs to work harder and can cause problems over time like increased blood pressure in the lungs, heart failure, or irregular heart rhythms. Closing a VSD will prevent these complications from happening.
Most of the time a VSD doesn't need to be repaired immediately after birth. Depending on the size and location, it may even close on its own. Your baby will be monitored by a pediatric cardiologist after discharge from the hospital to determine if your baby will require surgery. Some of the common symptoms that you will be watching for is increased work of breathing, decreased energy, especially for feeding (becoming too tired to finish the usual amount of food he/she takes) which can lead to poor weight gain, and/or sweating with mild exertion.
(Diagram of VSD)
Atrial Septal Defect (ASD)
An atrial septal defect (ASD) is a hole between the upper 2 chambers of the heart (the right and left atria). Some ASDs will close on their own, usually by the time the child is 2 years old. If they do not close, or they are causing problems, then they will need to be closed either by surgery or cardiac catheterization. An ASD allows blood to flow from the left atria to the right atria which increases the amount of the blood in the right side of the heart and subsequently an increased amount of blood going into the lungs. Overtime this can cause right heart failure because of the increased stress on the right side of the heart from having to pump extra blood and can cause damage to the blood vessels in the lungs called pulmonary hypertension.
(diagram of ASD)
Ebstein's Anomaly
Coarctation of the Aorta
Total Anomalous Pulmonary Venous Return (TAPVR) or Partial Pulmonary Venous Return (PAPVR)
Pulmonary Atresia
Truncus Arteriosus
Atrioventricular Septal Defect
Immature Lungs
There are 5 different stages of lung development that occur during fetal life: Embryonic (~week 4-8), Pseudoglandular (~week 5-17), Canalicular (~week 16-26), Saccular (~week 24-37), Alveolar (~week 36 to several years after delivery). Your baby starts out with the formation of the large airways: the trachea which is what starts at the top of your neck and then travels down into your chest where is splits into 2 branches, called bronchi, that go into the left and right lungs. Then each of these bronchi continue to branch into smaller and smaller airways (this mainly occurs in the pseudoglandular and canalicular stages) and eventually at the end of the smallest airways, little air sacs are formed called alveoli. Alveoli are what are responsible for exchanging gases most importantly oxygen and carbon dioxide.
What type of breathing machines are there to help my baby breathe?
Low Flow Nasal Cannula
This type of cannula is a thin plastic tube that delivers oxygen directly into the nose through two small prongs. This type of device is used when only a small amount of oxygen is required.
High Flow Nasal Cannula
This type of cannula is used when a baby need some pressure and maybe oxygen as well. It looks very similar to a low flow nasal cannula. It is used in babies who usually breath all on their own but may occasionally have apneas, or pauses in their breathing.
CPAP/NIMV
Picture of a baby with a mask in place that can deliver CPAP (continuous positive airway pressure) or NIMV (noninvasive mechanical ventilation. This type of breathing help is used when babies can do some of the breathing on their own but not all of it. The machine does some of the work for them, specifically helping them inhale with each breath they take.
Mechanical Ventilation
Picture of a baby with a breathing tube also known as an endotracheal tube (ETT for short). When babies are born very premature (<28 weeks gestation) there is an increased risk that your baby will need breathing support in the form of an ETT which is connected to tube that is then connected to the ventilator or breathing machine. This helps babies breath who are not able to do it on their own. It can also provide oxygen if needed.
Respiratory Distress Syndrome (RDS)
When babies are born premature, their lungs are not fully developed which can create problems with their breathing. Gas exchange occurs in the alveoli and preterm infants, depending on how premature, do not have many alveoli. This can cause several problems the most important of which is being able to get oxygen into their bodies and get rid of carbon dioxide. In order to be able to exchange these gases in the alveoli, they need to be open and not collapsed down. One way to think about this is envisioning the lungs as a bunch of grapes and the alveoli are the grapes. In order to effectively exchange gases the grapes need to be big and round and if they turn into raisins then they can no longer function well. How babies keep their alveoli big and round is by a protein called surfactant which is made by these alveoli. However, premature babies don't have the same number of alveoli as a term baby and they don't make enough surfactant.
Luckily, modern medicine has found a way to make surfactant so that it can be given to babies after they are born if they need it. When babies require surfactant after they are born, they are diagnosed with something called respiratory distress syndrome or RDS for short. This simply means that your baby did not make enough surfactant on their own to keep their alveoli open. Some babies only need 1 dose of surfactant, others may require more than 1. This is usually done within the first few days of life. Surfactant is given to babies through a breathing tube (endotracheal tube or ETT for short). Some NICUs are giving surfactant through something called an laryngeal mask airway (LMA) which is less invasive that an ETT because the LMA just sits in the back of their mouth whereas the ETT has to go through the vocal cords into the airway.
Pneumothorax
This can happen when there is damage to the lung tissue and air leaks out from the airways in the lungs into the space between the outside of the lungs and the chest wall. They can range from small to very large pneumothoraces. The larger they are, the more they will push on and compress the lung causing it to not work well. This can cause your baby to have problems breathing. To fix this, there is a procedure called a thoracentesis. This is where a small needle is inserted into the air space that is causing the problem and this enables that air to be taken out. Once all the air is removed, the needle is taken out. Usually this is all that needs to be done. However, if the air re-accumulates, then your baby may need a small flexible tube inserted into that space, called a chest tube, so that the air can be taken out on a continuous basis until the lung tissue can heal and stop leaking air into that space. Often a chest tube will stay in for a few days.
Long term complications
Chronic Lung Disease (CLD)/Bronchopulmonary Dysplasia (BPD)
Babies that are born very premature and have breathing problems requiring them to need support by either a breathing tube or by CPAP or other support device can develop BPD, sometimes also called chronic lung disease. This is very common for these babies to have this diagnosis. What is means is that your baby is continuing to need some type of support and/or oxygen after 36 weeks corrected gestation. Most babies do very well and don't need to go home on any respiratory support, but some still need oxygen and can be discharged with a low flow nasal cannula that can give them oxygen. Babies lungs are still growing and developing even after they reach term age which means that their lungs can grow and develop over the first few years of their life and grow out of their breathing problems. The best way to ensure that their lungs continue to grow in the healthiest way possible is to keep them away from second hand smoke, avoid visiting many people who will be in close contact with the baby to limit the risk of infections like colds, and make sure your baby stays up to date with their vaccines. If your baby who was born premature, even if they didn't need oxygen going home, they are more likely to have severe complications from a typical cold or flu than babies not born premature or older children or adults.
Jandice / Hyperbilirubinemia
Another name you might hear is "hyperbilirubinemia." This is a very common problem that premature, and even some term infants, have during the first 1-2 weeks of their life. Jaundice occurs when there is higher levels of bilirubin in your baby's blood than is normal. Your baby's skin will likely have a yellowish color to it. Your baby's medical team will order a blood test to see how much bilirubin is in your baby's blood and whether they need treatment.
Treatment
This is typically treated with something called phototherapy. This can happen in 2 ways, either placing your baby on a "biliblanket" which is a rectangular blue pad that when turned on lights up blue, or blue lights on stands that can be placed so that they are shining down from above on your baby. You baby will have little eye masks on to protect them from the light. This light is not harmful (it is not ultraviolet or UV rays like those that are in tanning salons or from the sun). These special lights only have a certain wavelength of light which is the exact wavelength needed to breakdown the bilirubin so that your baby can poop it out.
How will I know if my baby's bilirubin level decreases and is normal? Your baby's medical team may recheck the bilirubin level several times to make sure that the phototherapy is working. Some premature babies will need repeated treatments with phototherapy before their body is able to handle the bilirubin on their own.
Where does bilirubin come from?
The red blood cells in our bodies are made up of several things, one of which is something called hemoglobin. When the red blood cells breakdown (which is a normal process as your body constantly makes new red blood cells), this hemoglobin is released into the blood where is it taken to the liver and turned into bilirubin. Normally, you would then get rid of this bilirubin in your poop. However, premature infants often have trouble pooping regularly after they are first born which contributes to them having jaundice (or hyperbilirubinemia) and possibly needing treatment.
